
Gratitude, Growth, and Good Health
Changes in federal and state funding have required LifePath to adjust to urgent pressures by reducing program offerings. Unfortunately, LifePath’s Healthy Living Program, which has provided support and education for those in our community living with chronic conditions for over 15 years, has been discontinued. As the former Healthy Living Program Director, I want to

Keeping Your Brain Healthy
Lots of our Healthy Living participants are worried about memory and brain health. Our memory classes get filled immediately with older adults worried about forgetting names, faces, where they put things, etc. There is good news, however, because not only do our memory classes help, but many medical professionals describe how lifestyle changes can have

Keep Moving: How Regular Walking Can Help Prevent Falls
Staying active is important at any age, but it’s especially important as we get older. One of the best and easiest ways to stay active is walking. Walking regularly isn’t just good for your heart and muscles; it can also help prevent falls. Falls are a serious risk, especially for older adults. But with some

The Secret Joy of Aging: The Art of Retirement
As we have seen in national examples recently, it can be really difficult for those of us aging to decide when it is time to stop working. Some of us lose our sense of purpose and can get depressed and neglect our health. Others see retirement as a time to finally focus on ourselves, a

The Better Breathers Support Group at Baystate Franklin Medical Center
Are you suffering from lung disease, or know someone who is? Baystate Franklin now hosts a monthly Better Breathers Meeting in person.
The American Lung Association’s Better Breathers Club programs have connected people living with lung disease to educate, support, and help each other in communities around the country for over 50 years.
Better Breathers Club members

Education Isn’t Enough
The Healthy Living Department at LifePath serves people who are trying to make changes to improve their chronic condition. We must try to manage weight, avoid foods that make our conditions worse, figure out how to exercise, how to advocate for medical care, etc. Making these changes can be harder for some of us than

The Power of Peers
If the Healthy Living workshops at LifePath run by any core principle, it is, “We are all in this together.” Healthy Living workshop leaders, men and women with chronic conditions themselves, volunteer many hours facilitating workshops to support community members living with challenging health conditions.
Even though many come with professional backgrounds in nursing, health education,
Three Years of Work Culminate in Launch of Age & Dementia Friendly Action Plan
An Age & Dementia Friendly Action Plan is a comprehensive strategy developed by a community to ensure that its infrastructure, services, and policies are designed and implemented in a way that supports and accommodates the needs of people of all ages, particularly older adults. These action plans are specifically focused on creating environments that are

Communication and Living with Chronic Conditions
Living with chronic conditions affects our entire lives; we might need accommodations at work, or when we travel or shop, or gather with our friends. We need good communication to manage all this and help others to understand how they can help and support us. We need good communication to understand how our condition affects
May is Older Americans Month, a Time to Celebrate Aging Unbound and Challenge the Status Quo!
Established in 1963, Older Americans Month (OAM) is celebrated every May. Led by the Administration for Community Living (ACL), OAM is a time for us to acknowledge the contributions and achievements of older Americans, highlight important trends, and strengthen our commitment to honoring our older citizens.
This year’s theme, Aging Unbound, offers an opportunity to explore
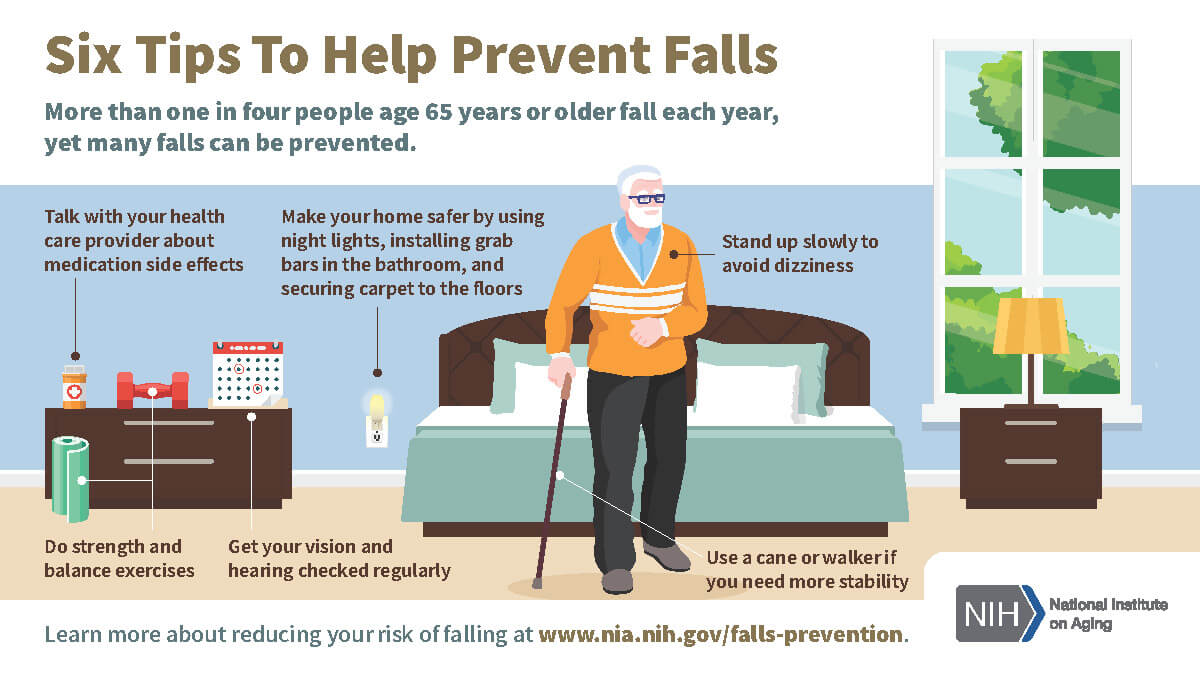
Older Adults and Balance Problems
Have you ever felt dizzy, lightheaded, or as if the room were spinning around you? These can be troublesome sensations. If the feeling happens often, it could be a sign of a balance problem.
Many older adults experience problems with balance and dizziness. Problems can be caused by certain medications, balance disorders, or other medical conditions.

Villages are Thriving Thanks to Resident Effort and Ingenuity
The vast majority of older people in Western Mass want to “age in place,” or continue living in their homes and communities for as long as possible. To achieve this goal, people can seek support from their local aging network. This includes Councils on Aging, senior centers, LifePath (an Area Agency on Aging), private businesses
